Benchmarking plan designs, premium costs, and employee contributions is one thing, but have you ever benchmarked the bones and infrastructure of your health plan? The things upstream that everything flows from? The foundation that your health plan is built on?
See, costs (and your upcoming renewal) are lagging indicators; but contractual freedom, leveraging data, and transparent relationships are all leading indicators.
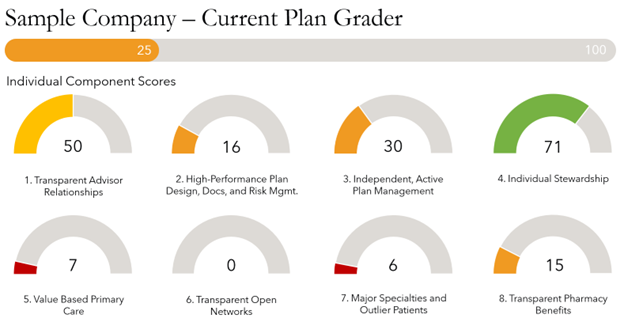
Enter the Health Rosetta Plan Grader™. An independent health plan assessment designed to evaluate the foundation of your benefits program. After years of research and curation, the Health Rosetta team has identified the 8 building blocks of a high-performing health plan.
Every health plan starts somewhere and most traditional ‘status quo’ health plans range in between 20-40 points (out of 100). While this is a gloomy start, it also points to the high potential and opportunity your health plan possesses.
For a brief introduction to the Plan Grader™ and the individual components keep reading.
#1 – Transparent Advisor Relationships
How much money is your broker actually making? Do they disclose all direct and indirect compensation?
Without knowing the answers to these two questions, it’s difficult to know who the broker is working for. Meaning there are a lot of mis-aligned incentives in broker compensation and this assessment helps ‘right the ship.’
#2 – High-Performance Plan Design, Documents, and Risk Management
High-performance can mean a lot of things, and in this instance, it refers to plan designs that optimize high-quality/low-cost providers, legal documents that are negotiated on your behalf, and taking ownership of your risk.
A key recommendation here is to hire subject matter experts to work on the health plan’s behalf in third-party administrator (TPA) and pharmacy benefit manager (PBM) contracts.
#3 – Independent, Active Plan Management
Do you own your ‘own’ data? Are you leveraging that data to make informed decisions?
Independent is the opposite of dependent; and if your health plan is dependent on the carrier or TPA for handling your data and managing who the health plan can and cannot work with, then your health plan is likely handcuffed and reactive.
#4 – Individual Stewardship
Are your employees empowered and educated to be stewards of the health plan as they enter in and engage the health care system?
The reality is the health plan’s annual spend is made up of all the individuals that use it; if they aren’t equipped to be good stewards, you might have a mess when the health plan pays the bill.
Invest in communications, education, and creating ownership of the health plan.
#5 – Value Based Primary Care
Sitting in a waiting room, seeing a doctor for 7-12 minutes, and then being sent for testing or to a specialist isn’t how primary care is supposed to be or how it’s been practiced for centuries. This ‘current’ phenomenon, built to herd patients through the system, is a biproduct of mis-aligned incentives and doesn’t serve your people well.
Value based primary care restores patient centric care and builds trust in the patient-provider relationship…which ultimately leads to better outcomes.
#6 – Transparent Open Networks
Navigating to an ‘In-Network’ provider is a form of steerage, but the price variance between Provider A and Provider B for the same service can be up to a multiple 10x. The problem is nobody knows the difference, there is ZERO transparency on prices.
In a transparent, open network, prices are what they say they are, ‘transparent’ and members can make informed decisions based on this.
Work to unlock the power of free market economics…it’s how we purchase all other goods and services, we should expect the same in health care too!
#7 – Major Specialties and Outlier Patients
Eighty percent of your claims are driven by 20% of your population, or some metric close to this. So how is your health plan supporting those most vulnerable to high costs and severe health needs?
There are more and more point solutions, businesses designed to help specific diagnosis or disease, coming to market each year. Using the aforementioned data (see #3) the health plan can make targeted investments to come alongside your population.
#8 – Transparent Pharmacy Benefits
It might sound like a broken record by now, but we will say it again (or three times)…transparency, transparency, transparency. If it’s not happening in pharmacy benefits, then we’re leaving meat on the bone.
Leveraging pharmacy consultants to run procurement, negotiate contracts, and audit PBMs is a huge value add and highly recommended.
The phrase, “I don’t know what I don’t know,” no longer has to be the case when it comes to assessing if your health plan is high-performing or not. The Health Rosetta Plan Grader™ provides you the information you need to know!
If you’d like to get your health plan’s Plan Grader™ please don’t hesitate to ask.

